AAC and Healthcare Professionals
PrAACtical AAC, a popular blog for speech therapists working in augmented communication, shared a post this morning that hit me hard. "No matter what the age or type of disability," it said, "almost all AAC learners face the challenge of communicating effectively during encounters with healthcare professionals. People with AAC needs are among those who are considered to be communication vulnerable and do best when there are planned supports in place."
Communication vulnerable.
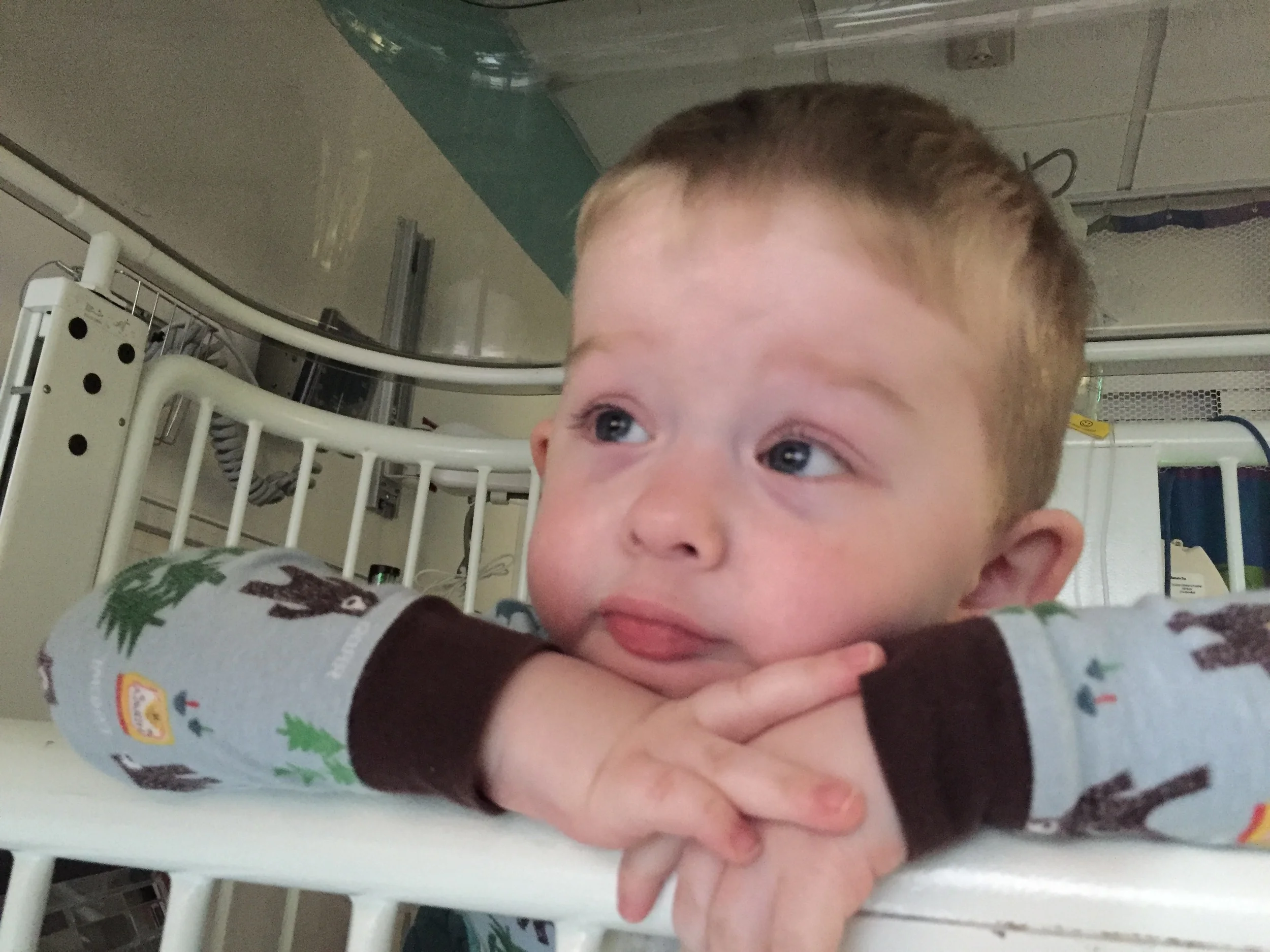
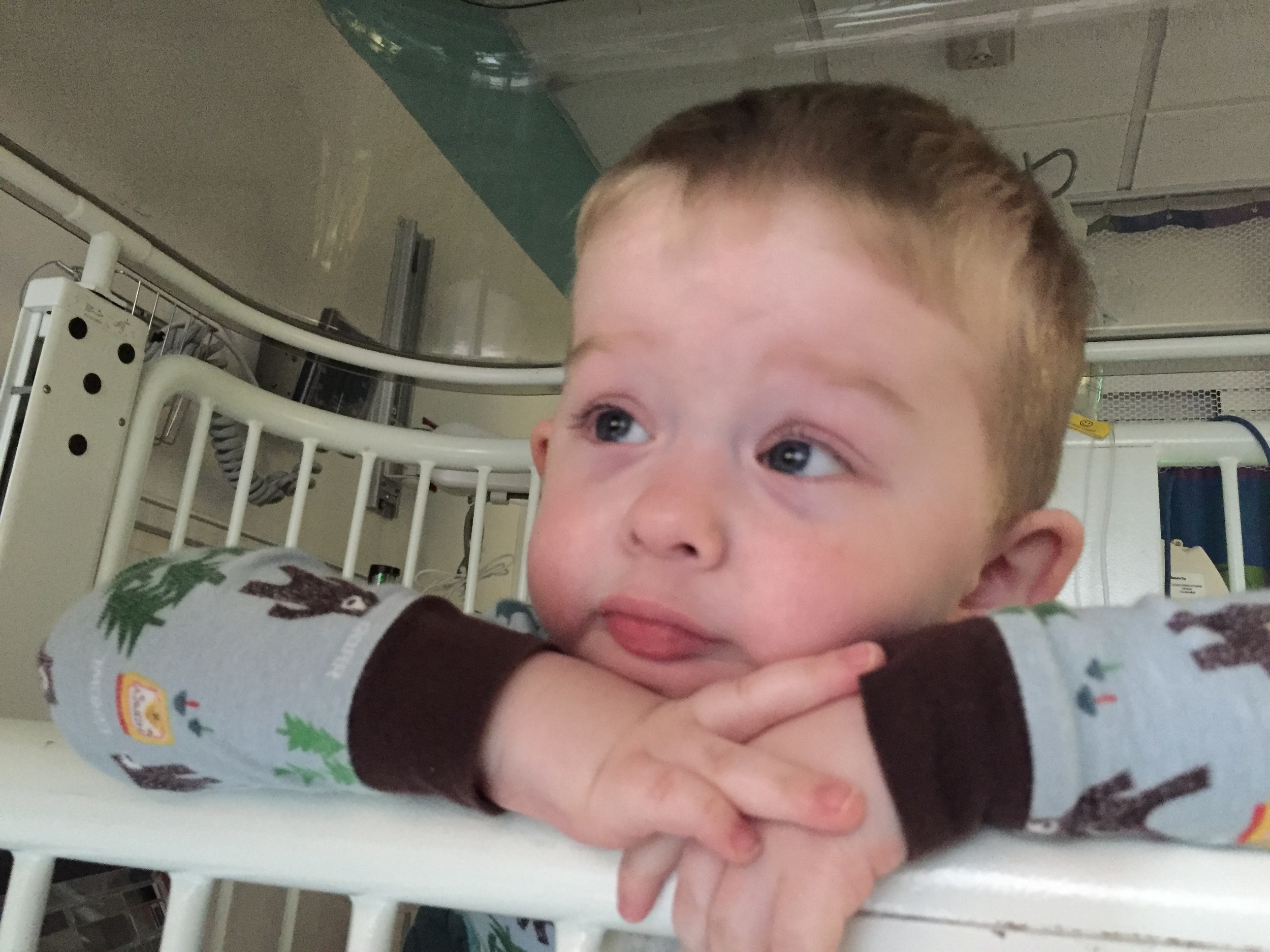
I live that existence with Nathaniel every time we interact with healthcare professionals.
A comment was made by a nurse during last week's hospitalization that revealed Nathaniel's vulnerability. A quick side note - I try very hard give health care professionals the benefit of the doubt and focus on positive interactions. I try to walk away remembering only the good things about our experiences. I have to. We have far too many interactions with healthcare professionals to continually dwell on the negative. I do not share the following experience to point a finger at any one nurse, department, or institution. I do share our personal experience to build on PrAACtial AAC's call for health professionals to be aware of and address the complex communication needs of their patients and for speech therapists help build bridges between patients and providers. Nathaniel's eight hospitalizations in the last eight months do not take into account the endless private duty nursing shifts, doctor appointments, therapies, and tests. In 2014, Nathaniel (and parents) had 734 appointments and interactions with healthcare professionals. An average of fourteen every week. When I calculated that number, hospitalizations were counted as one interaction. However, we deal with roughly ten to twelve different healthcare professionals every day that Nathaniel is a patient in the hospital. Nathaniel and parents had to navigate his complex communication needs with thirty new professionals last week on top of dealing with pain, fear, lack of sleep, hunger, and his illness.
It was in a moment of fear that a communication break down probably occurred between a nurse and Rich. After being awake all night with Nathaniel in the emergency department, Rich faced the challenge of admitting him to the floor for inpatient care while I went home to sleep a few hours. A last minute, unexpected decision sent Nathaniel to ICU due to a resident's concern that our son was becoming septic. New faces, needle sticks, bright lights, x-ray machines, loud voices, isolation gowns, and masks had Nathaniel on edge even before the move out of emergency. Terms like septic and ICU put Rich on edge. Communication skills were probably at an all time low for both of them. In the process of sharing information with new nurses, Rich hastily said something like, "Nathaniel can't talk."
Seven hours later when Nathaniel was repeatedly signing ALL DONE through a painful procedure, a nurse scolded him. "Stop waving your arms!"
Having returned with just two hours sleep and now sitting beside the crib, I rose, literally, to Nathaniel's defense. "He is signing ALL DONE. He is trying to talk to you."
Her next comment cut deep because it goes against everything I know to be true about Nathaniel. "He doesn't talk," the nurse informed me, "Dad told us that on admission."
Doesn't talk.
Doesn't talk.
It was like a kick in the gut.
At a surface level, she was correct.
My son does not talk in the typical way of vocal cord vibration and forming consonants and vowels sounds with his mouth, lips, and tongue.
But she was also extremely wrong.
My son does communicate.
He uses nonverbal communication, sign language, and an augmented communication device.
He has been communicating since the moment I met him when he looked from adoptive mom to foster mom for reassurance. He has been successfully using a dynamic speech generating app on an iPad since he was a year old. If there has been one area of priority to me personally and our family in caring for Nathaniel it has been to acknowledge that he is capable of and eager to communicate. To talk. We believe he has much to say. We listen. We respond. We believe that his talking - whether with his eyes, facial expressions, mouth clicks, hands, arms, feet stomping, or iPad - matters.
I understand the nurse's dilemma. She was given a bit of information quickly and when faced with the pressures of hospital routines and demands, she made assumptions. Assumptions that, honestly, sway things in her favor. If a healthcare professional assumes a patient will not attempt to communicate, their responsibility to listen is alleviated. Listening with speaking patients is hard. Listening to the voices of AAC patients requires more.
Rather than just identify the problem and complain about our experience, I want to offer three tips to healthcare professions when treating pediatric patients with complex communication needs and working with their parents:
1. Listen with your eyes.
My son makes no audible noise. You will not hear him cry sitting behind a computer at the desk in the middle of the unit surrounded by the chatter of your co-workers. You have to be near him. You have look up from your charting. You have to look at him. Watch his face; it tells you a lot. Watch us, his parents, interact with him. We are the experts in communicating with our son. Watch his body language and value it greater than you do when interacting with speaking children. When faced with a fearful situation, all children regress to more basic communication skills. Pulling away. Hiding under a blanket. Putting his hands over his eyes. These are my son's way of saying, "No, leave me alone. I am scared." The best thing you bring into the exam or hospital room is not your understanding of alternative methods of communication or devices, but your eyes. See him. Watch him carefully.
2. Ask questions.
Recently I took Nathaniel for a test that prevented having his talker close. One of the healthcare professionals in the room asked, "Mom, does Nathaniel use sign language and what signs might we expect to see during this test?" WOW! This woman entered the situation presuming competence and communication. She recognized her limited understanding of Nathaniel as a unique patient. She was humble enough to ask questions and be taught by a parent and child. Do all this. Presume competence and communication. Recognize your limited understanding of each patient. Be humble. Ask questions. Be teachable.
3. Engage longer.
I know. Communicating with my nonverbal child takes a lot of time. He is often slow at finding the right button on his talker. You do not know his signs and require me to translate. I can only imagine that while he is searching on his device or I am modeling his device language in your presence, that you are thinking of all the other patients and needs you have to deal with before you go home. The truth is augmented communication is harder than speaking. It requires more of everyone. More of my child. More of me. And more of you. We will cement our relationship as a team the harder we work together at communicating. He will learn to respect your medical expertise and help in relationship to how his nonspeaking voice is heard and respected.
Nathaniel is fortunate to be well supported by an AAC team who is committed to not only his language growth, but advocating for him with healthcare professionals. One of those ten people we interacted with on Wednesday before discharge was our therapist who delivered a sign to me. "Kim, keep this in your hospital bag. Post it on Nathaniel's door immediately upon arrival in Emergency or on the floor. Ask the nurses to make copies if you need them. Put another by his crib. Ask the floor staff to call for a consult with me so that we can talk with his nurses and doctors about Nathaniel's communication needs." This is how change will come for those who are communication vulnerable. One conversation. One healthcare professional. One at a time more people will learn to listen well.